Understanding the pathogenesis of SARS-CoV-2 encephalitis
In collaboration with an international team of scientists, HT researchers identified a missense mutation in a gene involved in brain-intrinsic immunity as the genetic cause of SARS-CoV-2 brainstem encephalitis. The findings are published in the Journal of Experimental Medicine.
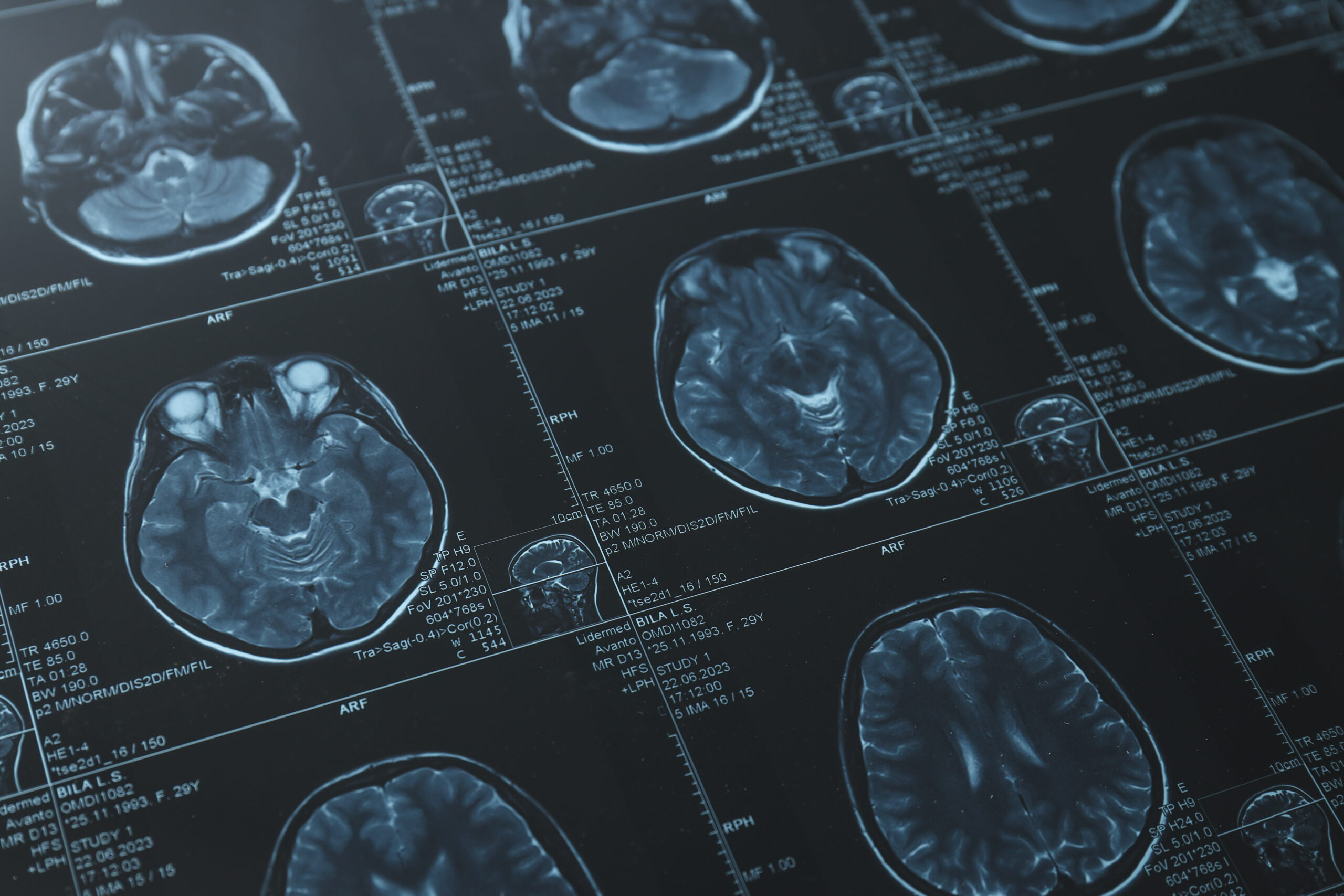
Severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) causes COVID-19, a respiratory illness responsible for the global COVID-19 pandemic in 2020. In addition to targeting the lungs where it produces severe respiratory problems, SARS‑CoV‑2 can enter the central nervous system, which includes the brain and the spinal cord, and lead to inflammation of the brain tissue or encephalitis.
The pathogenesis of SARS-CoV-2 encephalitis is poorly understood. To investigate the mechanisms of SARS-CoV-2 encephalitis, researchers from the Rockefeller University (USA), the Sloan Kettering Institute (USA), the University of Gothenburg (Sweden), Inserm, Paris (France), and the group of Oliver Harschnitz at Human Technopole (Italy), performed whole-exome/genome sequencing of 16 patients from the COVID Human Genetic Effort (www.covidhge.com) cohort who developed isolated encephalitis following acute SARS-CoV-2 infection. The sequencing allowed the researchers to identify a patient, a Swedish 14-year-old boy, carrying a missense mutation of the RNA lariat-debranching enzyme 1, DBR1(I120T).
DBR1 is highly expressed in the brainstem and spinal cord, where it removes byproducts of RNA splicing or lariats. DBR1 was previously reported as a genetic aetiology of brainstem viral encephalitis induced, for example, by Herpes Simplex Virus 1 (HSV-1), influenza B virus or norovirus. The I120T mutation is not deleterious per se but it lowers the protein level of DBR1 and thereby decreases RNA lariat-debranching activity.
The researchers found that fibroblasts from the patient contained low levels of DBR1 protein and high levels of RNA lariats. Similarly, DBR1 I120T/I120T hindbrain neurons generated from human pluripotent stem cells showed high levels of RNA lariats, which decreased when the wild-type version of DBR1 was overexpressed in such cells. Importantly, the team noticed that SARS-CoV-2 infection increased the levels of RNA lariats in both healthy and DBR1 I120T/I120T hindbrain neurons. Altogether, these findings suggest that SARS-CoV-2 infection is uncontrolled in DBR1-deficient hindbrain neurons due to the accumulation of RNA lariats.
“Our findings confirm that DBR1 is a gatekeeper of the human brainstem against several viruses, including not only HSV-1, influenza B virus, and norovirus, but also SARS-CoV-2. Patients with DBR1 deficiency should be vaccinated, not only against SARS-CoV-2, but probably also against a broader range of viruses”, the authors say.
Oliver Harschnitz, co-last author of the study, also commented “It will now be important to decipher the detailed molecular mechanisms by which the accumulation of intronic lariats impairs cell-intrinsic immunity to viruses in the brainstem. Such studies may pave the way for developing effective preventive or therapeutic measures for patients prone to brainstem encephalitis.”




