Shedding light on the molecular mechanisms of Gabriele-de Vries Syndrome

Using advanced stem cell models, Human Technopole researchers show how mutations in the YY1 gene cause widespread dysregulation of genes crucial for brain development in multiple cell types, leading to structural abnormalities and impaired neuronal function. The results of the research are published in the Nature Portfolio journal Molecular Psychiatry.
Gabriele-de Vries Syndrome (GADEVS) is a rare neurodevelopmental disorder caused by mutations in the YY1 gene encoding for a transcriptional regulator that can either repress or activate the transcription of various genes. Individuals with GADEVS exhibit developmental delay, intellectual disabilities, craniofacial abnormalities, and skeletal and cardiovascular issues, among others. Despite growing recognition of this condition, the molecular mechanisms underlying its symptoms remain largely unknown.
The group of Giuseppe Testa at Human Technopole, which had first characterized GADEVS in 2017, filled this gap in collaboration with several research teams worldwide by analysing the cellular and molecular changes underlying this condition and uncovering how YY1 mutations disrupt early brain development.
Using patient-derived induced pluripotent stem cells (iPSCs), the researchers observed that cells carrying YY1 mutations displayed broad transcriptional downregulation, suggesting that many crucial genes were not activated in YY1 mutant cells. This finding was consistent across different types of mutations (truncating and missense mutations), indicating that reduced YY1 activity is a key driver of the disease.
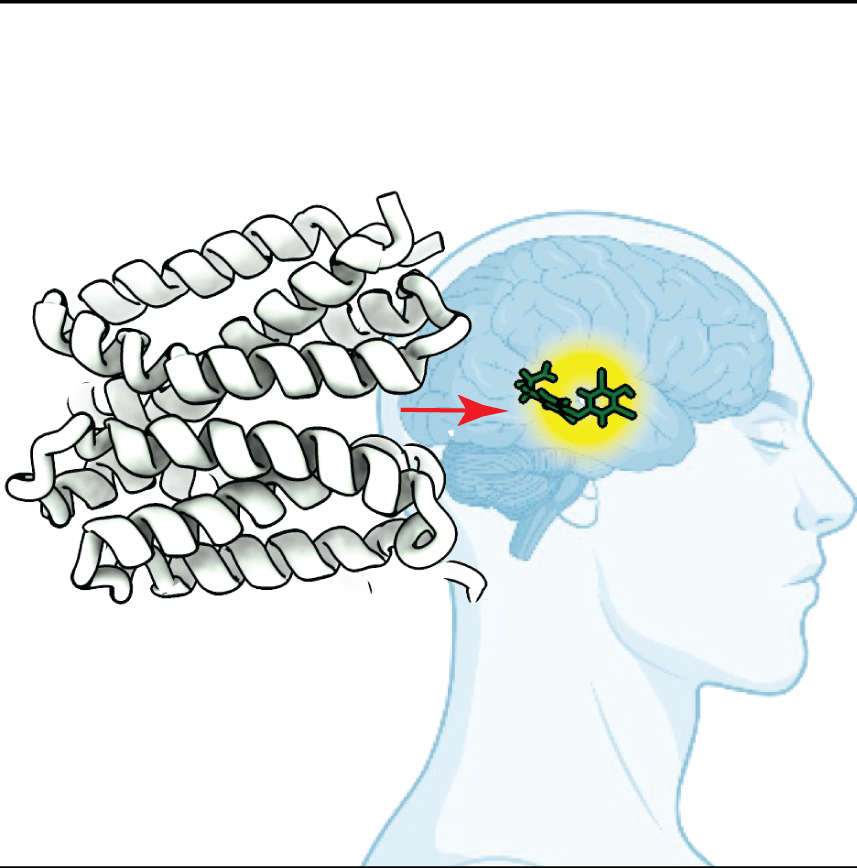
To model early brain development, the group grew brain organoids – in vitro tridimensional models recapitulating salient aspects of the developing human brain – and discovered that organoids from GADEVS patients presented abnormal ventricle-like structures, which mimic the brain’s fluid-filled spaces. These abnormalities closely resemble ventricle atrophy observed in GADEVS patients. As the brain organoids developed, specific groups of neural progenitor cells – the cells that eventually become neurons – showed signs of misregulation. In particular, Testa and collaborators found that the differentiation of intermediate progenitors, a key cell type in brain development, was impaired. In addition, researchers observed that several genes related to synaptic function were disrupted, thus potentially explaining intellectual disabilities observed in GADEVS patients. The teams then focused on astrocytes – specialised cells that support neurons – and found that these cells respond abnormally to YY1-deficient neurons. They observed a strong inflammatory reaction, characterised by the activation of genes linked to immune response closely recalling gliosis (excessive inflammation in the brain), which is often observed in GADEVS patients, and could thus be tracked to specific genes and potential targets of intervention. This suggests that GADEVS affects neurons and triggers harmful cross-talk between different brain cell types, potentially worsening neurological symptoms. Finally, researchers explored gene regulatory networks and identified a dysfunctional interaction between YY1, NEUROG2, and ETV5 genes, the latter being critical for guiding brain development. They found that this network is disrupted in GADEVS, leading to widespread developmental abnormalities. Interestingly, they also detected a cellular feedback mechanism attempting to compensate for the loss of YY1, but it appeared insufficient to fully counteract the effects of the mutation.
In summary, these findings significantly advance our understanding of GADEVS by demonstrating how YY1 mutations cause developmental defects at the cellular, structural, and molecular levels. Importantly, it also highlights potential therapeutic targets, not only in terms of restoring YY1 activity to tackle the severity of developmental defects but also by potentially targeting the inflammatory response in astrocytes to mitigate some of the neurological alterations.
More broadly, the research emphasises the importance of gene regulation in brain development and highlights the value of stem cell-based models in studying rare disorders, paving the way for more personalised medicine approaches in the future.
By identifying key pathways involved in GADEVS, this study deepens our understanding of this rare condition and provides valuable insights into other neurodevelopmental disorders that share similar mechanisms.
Pereira, M.F., Finazzi, V., Rizzuti, L. et al. YY1 mutations disrupt corticogenesis through a cell type specific rewiring of cell-autonomous and non-cell-autonomous transcriptional programs. Mol Psychiatry (2025). https://doi.org/10.1038/s41380-025-02929-x
Image credits: Marlene F Pereira (Testa Group). The image shows human neurons (green) and mouse astrocytes (purple) cultured together in vitro to study neuronal maturation and astrogliosis.